Altitude Adaptation, Health & Ability To Train
The Highs & Lows of Altitude Training - Part Three
Part One, Introduction
Part Two, Oxygen Dynamics
A Summary of Oxygen Dynamics
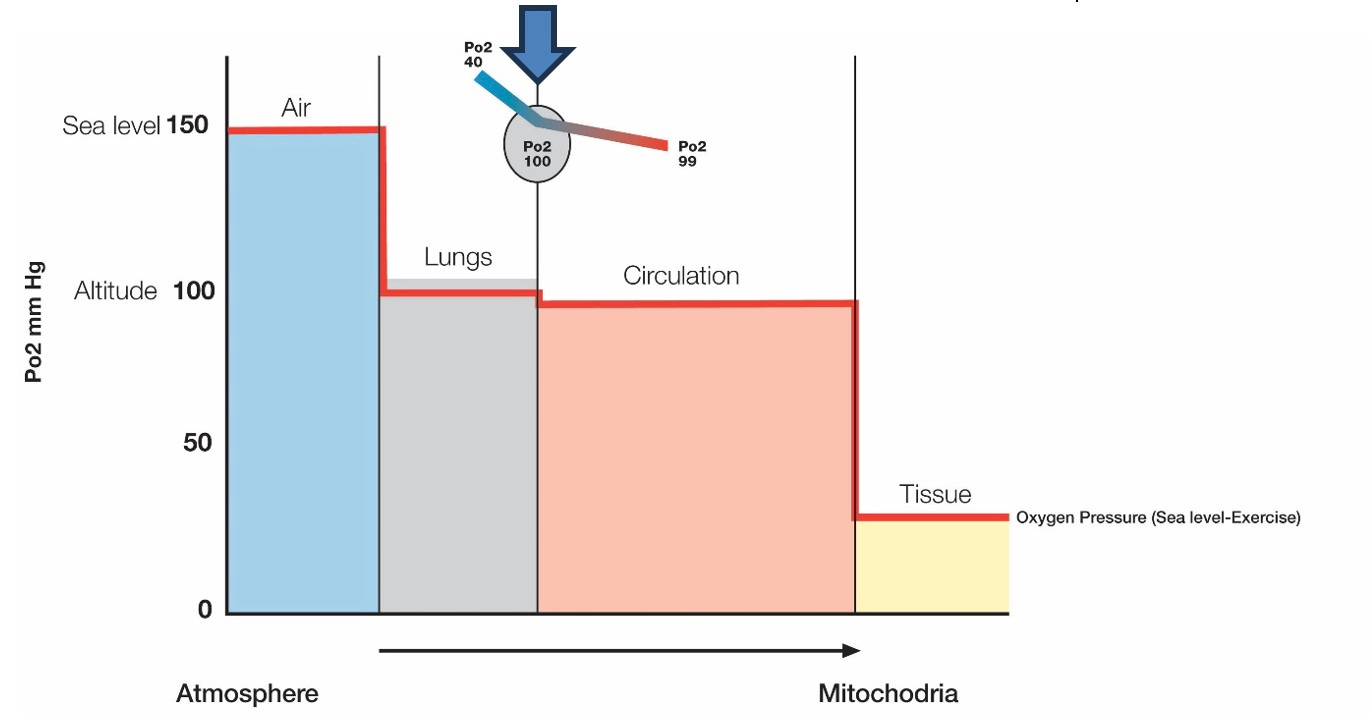
Our previous article discussed the mechanisms of transporting oxygen from the external environment to the energy-producing mitochondria within muscle cells. We highlighted the significance of a substantial pressure gradient between the partial pressure of oxygen in the outside air (159 mmHg) and within the mitochondria (10-20 mmHg). This allows oxygen to diffuse down the pressure gradient, called the oxygen cascade (Figure 1).
Figure 1: The oxygen cascade at rest at sea level. Notably, when the oxygen-depleted venous circulation returns from the muscle tissue and reaches the lung via the pulmonary artery, the PaO2 is 40mmhg, which creates a significant pressure gradient to assist the diffusion of oxygen from the lung into the circulation. By the time the circulation leaves the lung (via the pulmonary vein), it is rich in oxygen, and the PaO2 has risen to 99mmhg (blue arrow).
Active inhalation adds to getting the air deep inside the lungs before it diffuses into the circulation. Oxygen is transported in the bloodstream, bound to a protein called haemoglobin in red blood cells. At sea level, 98-100% of haemoglobin gets saturated with oxygen at rest. This can be measured with a pulse oximeter and is expressed as SpO2 (oxygen saturation in the blood as measured by a pulse oximeter). SpO2 is directly related to the PaO2 in the blood, which is much more challenging to measure.
The enzyme 2,3-DPG plays a crucial role in releasing oxygen from haemoglobin when reaching its destination, enabling its diffusion into the muscle cells. Once oxygen reaches the muscle cell’s fluid, it is conveyed to the mitochondria by a transport protein called myoglobin. From there, it diffuses into the mitochondria, where it is utilised for energy production.
When ascending to higher altitudes, the pressure of the ambient air, and consequently the partial pressure of oxygen in the air, decreases with increasing heights. This causes the air to become ‘thinner’. The same amount of air at altitude contains fewer oxygen molecules than at sea level. This results in a drop in PaO2 and, therefore SpO2, called hypoxia (a lower-than-normal oxygen concentration in our blood and body tissues).
Pulse Oximeter
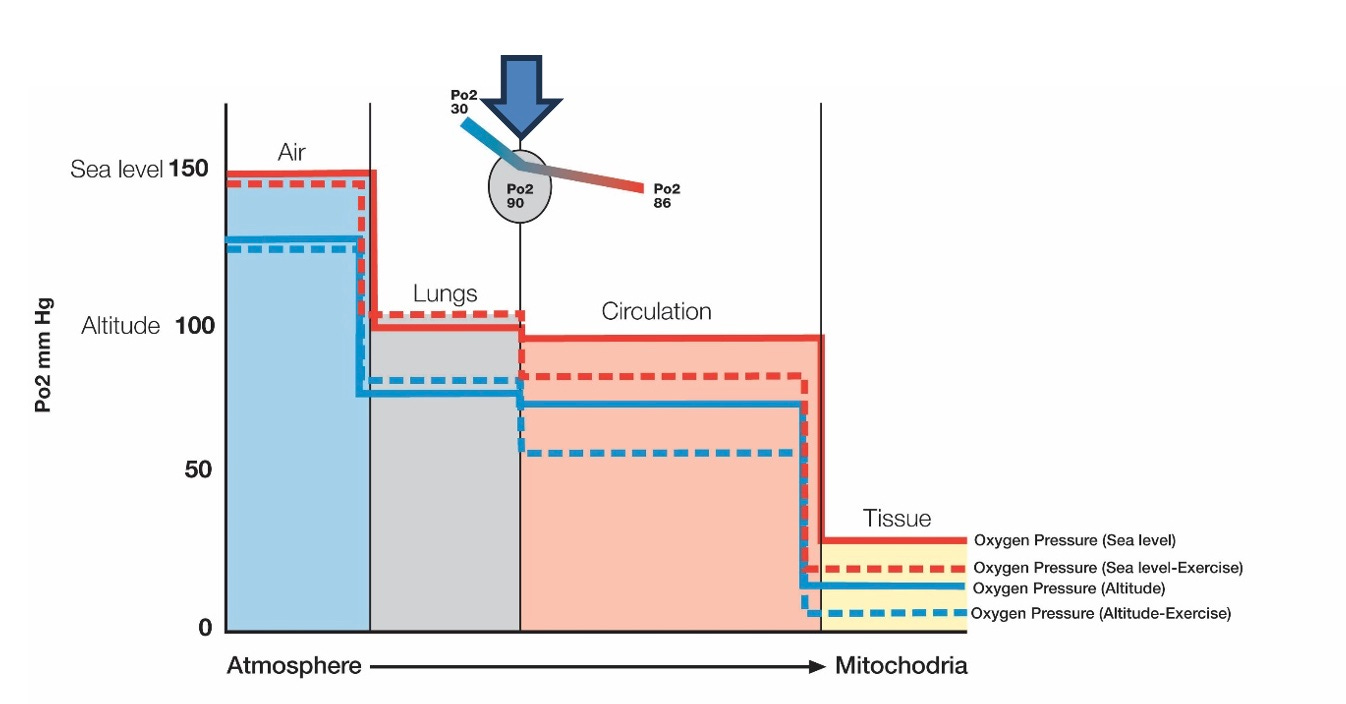
The pulse oximeter measures the level of hypoxia in the circulation. This device fits at the end of your finger and calculates the oxygen concentration in the blood (SpO2) by measuring its colour. Oxygen-rich blood is bright red. It turns a darker red when less oxygen is circulating (hence the colour difference between arterial and venous blood). When exercising at sea level, the SpO2 drops from its resting rate of 98-100% to 92-97%, depending on the intensity of the exercise, as oxygen is sucked out of the circulation at a higher rate by the working muscles. The same happens when we exercise at altitude, where our SpO2 is already compromised. Our SpO2 can drop below 80% when we train at altitude, causing significant hypoxic stress.
Figure 2: A schematic representation of the oxygen cascade at sea level and altitude during rest and exercise. At altitude, at rest, the PaO2 of the returning venous circulation entering the lungs has dropped to 30mmhg (compared to 40mmhg at sea level) and has risen to 86mmhg (compared to 99mmhg at sea level) by the time it leaves the lungs, comparable to a SpO2 of 90-96% (blue arrow). When exercising at altitude, a further drop in SpO2 occurs due to the increased demand for oxygen by the muscle cells downstream. Note that this is a schematic presentation and that individual variations in SpO2 response at altitude and during exercise can differ significantly.
There is a promising technological development in muscle oxygen monitoring. A muscle oxygen sensor is a device that you place onto a working muscle. It measures how much oxygen is available at the cellular level. It is still experimental but may become a popular training monitoring device in the future.
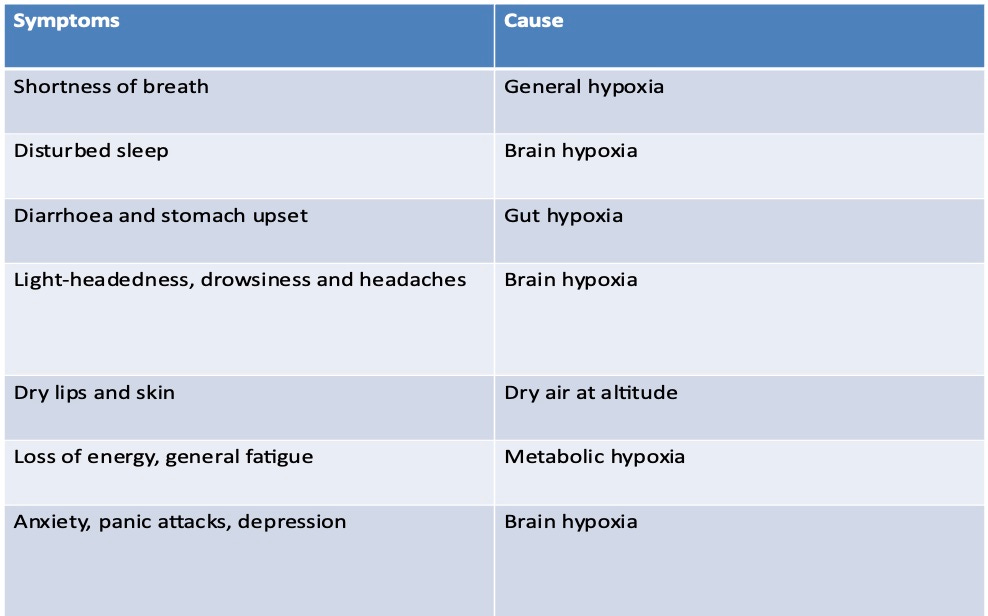
Altitude Sickness
A wide variety of physical and psychological symptoms can affect us when we are exposed to a hypoxic environment at altitude. Most of us experience one or more of these symptoms to some degree when we venture above 1000 meters. The symptoms become more severe the higher we go. Altitude sickness is a feared phenomenon amongst mountaineers as severe forms can quickly result in death. Symptoms are caused by a suboptimal supply of oxygen to our body tissues. The more common symptoms are summarised in Table 1.
SpO2 Monitoring
Besides subjective perception (how you feel), the pulse oximeter is the most crucial physical monitoring device at altitude to measure the hypoxic stress the body is under. Most pulse oximeters display SpO2 and pulse rate. Our pulse rate goes up when SpO2 drops. There are significant differences in SpO2 levels between individual athletes at altitude. Lower SpO2 levels are more likely to result in symptoms of altitude sickness. Figure 3 shows the relationship between oxygen saturation in the blood and the degree of physical and mental impairment. Individual variation in SpO2 is significant and indicated by the vertical black lines.
Figure 3: the relationship between SpO2 and altitude. (Adapted from McFarland 1972)
It is clear that when SpO2 levels drop below 85% for more extended periods, symptoms will be significant enough to interfere with wellness and the ability to train properly. According to the graph, this occurs at an altitude above 2400 meters, although individual differences in SpO2 response must be considered. Current research and coaching experience suggest that the best balance between physiological adaptation, athlete well-being and training ability appears to be between 1500 and 2500 meters (5000 to 8250 feet).
Altitude Classification
Table 2 divides altitude into seven distinct (but overlapping) levels, indicating how our health and training ability is affected.
Levels 1-3 are considered the compensatory zones. Here most people will adapt fully to the effects of altitude within a few days.
Level 4 is considered optimal for adaptation, but training at this level is compromised, and there is an increased likely hood of side effects like illness.
Levels 5 and 6 are considered de-compensatory, meaning that over time, the body will adapt insufficiently (level 5) or decompensate altogether (level 6).
Adaptations
The body employs various compensatory mechanisms to counteract the reduced oxygen delivery to the mitochondria. Five mechanisms aim to improve oxygen delivery to the working muscles:
The Lungs
The Heart
Blood Circulation
The Muscle Cells
The Metabolism
1) The Lungs. The rate of ventilation (breathing) increases. It is believed that athletes who experience a significant increase in breathing rate respond better to altitude training compared to those who don't. An increase in ventilation immediately improves SpO2. Animal studies have shown an improvement in diffusion capacity in the lungs, primarily due to an increase in the surface of the tiny air sacks deep inside the lung (alveoli), with also an accompanying boost in the small blood vessels (capillaries) that surround the alveoli and which receive the oxygen.
2) The Heart. The heart responds by increasing cardiac output through an elevated heart rate. This accelerates the transport of oxygen to the cells. However, over time at altitude, total cardiac production decreases for reasons that are not yet clear. This decrease in cardiac output has a detrimental effect on performance since relatively less blood can be circulated at any given moment.
3) Blood Circulation: The production of haemoglobin and red blood cells increases, enhancing the oxygen-carrying capacity of the blood circulation. Initially, the rise in haemoglobin concentration in the blood is due to a decrease in total blood volume. During the first few days at altitude, there is a noticeable increase in urination, which results in a relative state of dehydration, causing this decrease in blood volume. It is only later that additional red blood cells (erythropoiesis) are produced. This is stimulated by an increased production of erythropoietin, a hormone produced by the kidneys. Additionally, there is an increase in the production of 2,3 DPG, the compound that enhances oxygen unloading once it reaches its destination. It's worth noting that there appears to be a specific altitude and exposure time threshold required to generate a response in erythropoietin production. Scientists have established that a minimum height of 2100 meters (some suggest 2400 meters) with at least 300 hours of exposure is necessary to guarantee an increase in red blood cell and haemoglobin production. However, there are significant individual differences, as some athletes may produce new red blood cells at lower altitudes, while others require higher altitudes to achieve this particular adaptation.
4) The Muscle Cells: There is an increase in intramuscular myoglobin to maximise oxygen transport within the muscle cells to the mitochondria. Some studies have also shown an increase in the formation of small blood vessels (capillarisation) around the muscle cells, supporting improved oxygen delivery to the muscles. Furthermore, the number of mitochondria within the muscle cells and the amount and activity of aerobic enzymes that assist in energy production increase.
5) The Metabolism. There has been significant speculation in the literature regarding the mechanism and potential benefits of an increase in buffering capacity within the muscle cells at altitude, which occurs through a complex process. Another reported metabolic adaptation is a possible increase in fat utilisation, although the exact mechanism behind this is unclear.
The science behind these adaptations is complex and rooted in molecular biology, which is beyond the scope of this article. In short, there is a solid genetic determination of how our physiology responds to altitude, like how our bodies react to training. We all have a unique genetic makeup which regulates our physiology when we put our bodies under physical or environmental stress. Our genes send out continuous signals supporting our bodily functions to help us adapt and survive. These signals are unique to the individual, meaning we have our typical response to altitude exposure to the extent that scientists distinguish between ‘responders’ and ‘non-responders’. The ‘responders’ show obvious performance benefits following a stint at altitude, while the ‘non-responders’ show no or even adverse effects.
Responders Versus Non-Responders
We have learned through practice that the terms ‘responders’ and ‘non-responders’ are relative and manipulating and individualising the level of altitude (the hypoxic dose) and the type of training; most athletes can be turned into responders, even if some will respond more strongly than others.
American distance running coach Terrence Mahon introduced the concept of slow versus fast responders, depending on the athlete’s physiological makeup. He noticed that more aerobically inclined athletes respond well and can train without too many limitations at altitude. In contrast, the more anaerobic athletes are slow responders, and care must be taken with higher intensity training at higher altitudes with this group of athletes. In my experience, aerobic athletes desaturate less than anaerobic athletes at altitude, which fits in with Coach Mahon’s observations.
At this stage, finding the right attitude and training for the individual athlete is done mainly by trial and error. In the future, we can likely be more accurate in our prescription of altitude training through monitoring and genetic testing.
The Red Blood Cell Response
Scientists have been obsessed with the red blood cell response to hypoxic (altitude) exposure. For a long time, it was thought that there was a direct relationship between the increase in red blood cells and a positive performance response to altitude training. If you did not show increased red blood cells, you wasted time with altitude training and were classified as a non-responder. Other adaptations and their potential effect on performance were not considered. Increasing knowledge about the oxygen processing mechanisms and the adaptations occurring at altitude has made us realise there is more to it than just the red blood cell response. Every step in the adaptation process can contribute to improved processing of oxygen and, therefore, endurance performance.
Adaptations Over Time
Acute adaptations happen in the first few days of altitude exposure, gradually improving SpO2 readings at rest and during training. Most of the transformations are completed by days 7-10. This results in an improved ability to train.
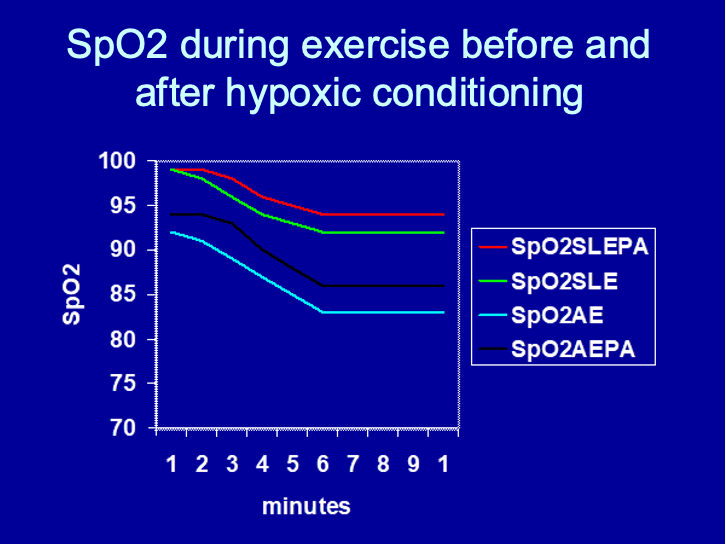
Figure 4 illustrates SpO2 levels during a 10-minute submaximal cycle test before, during and after altitude exposure.
The green line shows SpO2 from the test done at sea level, before altitude (SLE=sea level exercise).
The blue line represents the same test on day 2 of altitude (AE=altitude exercise).
The black line shows SpO2 done after three weeks at altitude (AEPA=altitude exercise, post altitude).
The red line shows the test results when returning to sea level (SLEPA=sea level exercise, post altitude).
What is most striking is the improved preservation of SpO2 during exercise following a stint of altitude training, not only at altitude (Black Line) but also following a return to sea level (Red Line), proving improved oxygen dynamics and successful adaptation.
It is clear from the above that understanding SpO2 monitoring is crucial to making altitude training work. Now that we have that understanding, we can discuss what this means for applying altitude training in the following article.